In my earliest caregiving days I didn't identify with the word. It's only in retrospect I understand that I was a caregiver.
It began with the very sudden death of my stepfather. He was ten years younger than my mother, who at the time of his death was 90. He was her caregiver. She was still quite independent and wanted to stay in their home so we hired someone to come in several days a week and help with groceries, cleaning, prepare some meals, take her out to lunch, etc. But she was devastated by his loss, had heart problems, and was almost blind with macular degeneration. She needed attention and help. As the months and years passed she found her way. Unfortunately her heart problems put her in and out of the hospital every few months and though she had lots of friends, she needed me to manage her medical care, doctors appointments, finances, and emergencies. It changed my relationship with her.
Then the death of my brother-in-law put me in the same situation with my sister. My sister has some dementia and is bipolar and lived in my town. Her husband was her caregiver. When he died it was up to me (and also my brother who was out of town) to figure out her care. We arranged for someone to come in several times a week to handle her pills and groceries and take her out. But it was my job to handle doctors, prescriptions, interactions with agencies and problem solve in regular and emergency situations, and also to visit. It changed my relationship with her from baby sister to manager.
Managing those sets of needs, along with being a business owner and wife was pretty stressful. Then came my husband.
My husband Larry has a progressive, terminal neurological disease. He’s recently been told by the neurologist he’s at “end stage,” whatever that means. It started around 2010.
He had some weird symptoms at first. Panic attacks. Some falls. Pain in his left shoulder and a weakness in his left arm - it trembled when he tried to lift things. I noticed his smile seemed different.
First they said it was a slightly torn rotator cuff and he had surgery and physical therapy. He still had the tremble and weakness which was attributed to unsuccessful therapy so more PT at another facility was prescribed. With no improvement, he was sent to a neurologist who said “I’ve got good news and bad news. The good news is it is not Parkinson’s Disease. The bad news is you have essential tremor, and we can’t do anything.”
His primary care doctor thought there might be something that could be done and sent him to another neurologist who did more tests and suggested it might be one of his cervical vertebrae. Traction was prescribed. Still no improvement. A physiatrist thought it was something similar to but different from essential tremor.
After two years of this, a friend arranged for us to see a movement disorder specialist in Boston who did surgery for essential tremors. We drove up with great hopes that we were on our way to answers and a cure. We planned a celebratory lunch in town. After an hour plus diagnosis, the specialist said that yes in fact it was definitely Parkinson’s. He was diagnosed on August 22 2012. I’ll always remember that date.
With no prior thought that PD was a diagnosis we were facing, we sat in shock. I remember the doctor talking on about medications and research trials as tears ran down our cheeks. We couldn’t hear her. Our world had changed. She called in the social worker.
But Parkinson’s wasn’t the end of the diagnosis. He had started without PD meds because he was in a Michael J Fox Foundation research trial. Then after a year he started on medication. After another year we realized his response was very different than others we met. They changed meds. Another alternative doctor thought it might be Lyme's Disease and low testosterone .He went on intense antibiotics and hormones. He had an awful time with side effects. His primary care doc said forget the alternatives. His neurologist changed his meds again.
By then we had moved my mother to assisted living and sold her home. Though she didn't want to go live with "all those old people" she made lots of new friends and enjoyed herself. Another hospitalization ended with a month of trying to fight the dreaded C-diff bacterial infection. She finally opted to stop her meds She moved into a lovely hospice house and after only 5 days she passed away. She had just turned 96.
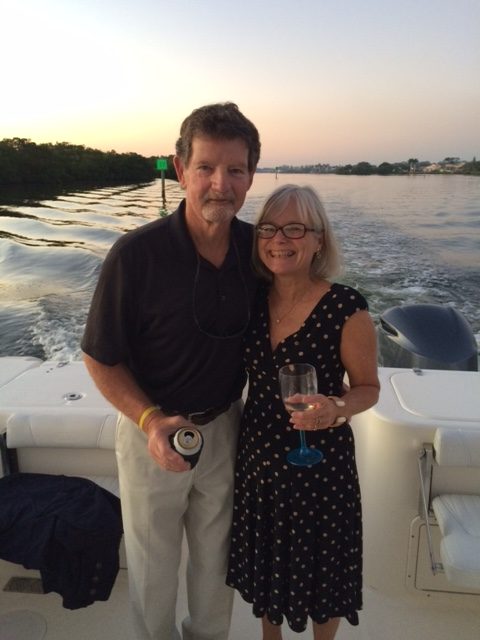
The following year, my husband could no longer work and closed down his business. The winter was brutal, more so for him. My business was portable so we decided to move to Florida to get away from the cold, thinking we still had many years together. We assumed we'd go back and forth to Massachusetts and kept some of our winter clothes. My brother found an amazing caregiver for my sister so I felt comfortable, though a bit of a deserter, leaving her behind.
We found a lot of support for Parkinson's Disease in Sarasota. Exercises classes. Support groups. I remember going to a support group for caregivers and thinking "I'm not a caregiver."
He kept complaining to the new doctors about the meds not working much. The doctors started to suggest he might not have Parkinson's but something called Parkinson Plus. After six months the new neurologist finally said “Maybe it’s ALS, I’ll schedule some tests.” Just like that our world got worse.
We went back to his neurologist in Boston so she could evaluate him. Three months later the nerve tests did not reveal signs of ALS. She suggested it might be MSA - Multiple System Atrophy, but there was no way of being sure without an autopsy. We opted not to have that test at that time. Ha, ha, ha.
Now, six years later, I’ve decided to keep a blog. I understand now that many of these progressive neurological diseases cannot easily be diagnosed at early stages. It is only as the disease progresses that the symptoms start to provide clues.
It appears my husband does in fact have Multiple System Atrophy, although we are still not sure. What we do know for sure is that he has a disease for which there is no cure, that progressively robs him of his life. We cannot slow it down. We can only learn to live as well as we can with it. Though it is his disease, it has become our life.
I go through anger, and denial. I go through feeling a victim and feeling a martyr. I go through feeling alone, and wanting to be alone.
I have no great aha’s or wisdom to offer, but a desire to share the journey, in the hopes that someone can be helped by what they read - that some benefit can come from all that we experience .