 Part 1 and Part 2 of my perspective on the healthcare professionals with whom we engage was from my point of view and today I want to present respite care from the patient’s viewpoint. Larry went into respite care for five days so I could get some good nights of sleep and some time to restore. He was willing although not thrilled about going. “I had to psyche myself up before I went,” he said today.
Part 1 and Part 2 of my perspective on the healthcare professionals with whom we engage was from my point of view and today I want to present respite care from the patient’s viewpoint. Larry went into respite care for five days so I could get some good nights of sleep and some time to restore. He was willing although not thrilled about going. “I had to psyche myself up before I went,” he said today.
Overall, his experience mirrored mine in some ways – they are mostly set up for bed bound patients. He said “it was so quiet – too quiet. I was the only one out of my room.”
“The food was pretty good,” he said. “I could have an ice cream sundae whenever I wanted.”
“Most of the nurses were good, but one didn’t listen to me.” That particular nurse didn’t listen to his explanation about how to use his catheters and made it more complicated and less comfortable for him. (I had been told they mostly see indwelling catheters, not the disposable straight catheters we use.)
She also didn’t listen when he told her there were two parts to his Bi-Pap machine face mask. She started with only the hard plastic part that attached to the tubing and didn’t use the part that goes against his face with the soft silicone gasket. So by the time she realized what was wrong, he had a cut on his nose from the plastic.
I couldn’t figure out why his hair looked so bad when he came home until he told me they’d only given him one shower in the five days and even then they only put water on his hair with a washcloth, they didn’t wash it with shampoo. Plus they only shaved about an inch on each cheek and left the rest of his face to go to stubble.
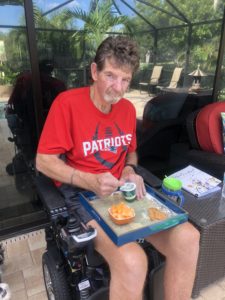
He ate all his meals alone at the dining table in the common room. Two musicians played the first day and he was the only one listening. The volunteers were great, but overall it was just too depressing.
I just asked what would have made it better. “Not going,” he said. “It was a place where people go to die. People were crying. There were rooms with whole families surrounding the patient. There was a group of about 20 people that took pictures in the common room. I was probably in their picture.”
That’s my Larry – photo bombing someone’s funeral picture.
In retrospect, we intellectually know that’s what a hospice house is for. It’s to take care of people at the very end of their lives. We should have expected what he experienced in respite care. But the social worker and the nurse were SO encouraging. They led us to believe it would be fine, he’d even enjoy it. They didn’t talk about how different a situation he was in from the other patients. That’s where the disconnect was.
 I did get some good sleep. I also painted our dark family room a light color and we’re both enjoying the new look. I feel so loved that he was willing to endure the respite week to take care of me.
I did get some good sleep. I also painted our dark family room a light color and we’re both enjoying the new look. I feel so loved that he was willing to endure the respite week to take care of me.


 Seems like every few months we run out of good days and I get overwhelmed – the tight ‘I can’t do this anymore’ feelings. Then something happens that loosens me up. It happened again this week.
Seems like every few months we run out of good days and I get overwhelmed – the tight ‘I can’t do this anymore’ feelings. Then something happens that loosens me up. It happened again this week.